Enkel – Soft tissue impingement
Als onderdeel van de specialisatie MSc. Strength and Conditioning (St Mary’s University, Twickenham – London) heb ik het onderstaande stuk geschreven betreffende ‘Soft tissue impingement van de enkel’. Dit is een blessure waarbij je een pijnlijke, gezwollen en aanzienlijk beperkte enkel kunt hebben. Bijvoorbeeld als gevolg van een verzwikte enkel en het houdt verband met chronische enkel instabiliteit en wordt ook gezien bij mensen met een osteochondraal defect. Het kan een complexe en aanhoudende klacht zijn welke per client specifiek in kaart moet worden gebracht. Kracht- en coördinatietraining tijdens de revalidatie is een aangetoonde methode om de klachten positief te beïnvloeden.
Soft tissue impingement of the ankle
Conservative treatment options and the application of current concepts in strength & conditioning and manual therapy to optimize rehabilitation.
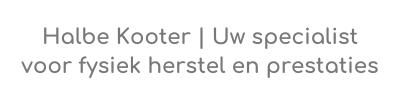
Soft tissue impingement (STI) is characterised by a mechanical and painful limitation of the ankle in anterior or posterior direction due to pathological contact between structures (Carreira & Ueland, 2020; Hess, 2011; Nery & Baumfeld, 2021). STI can contribute to chronic ankle pain and is part of broader impingement pathologies, together with osseous impingement and neuropathic entrapment (Shane et al., 2016). Anterior STI can be subdivided into synovial scar tissue formations, menisoid lesion formations and impingement of the distal fascicle of the Bassett ligament (distal fascicle of the anterior inferior tibiofibular ligament), figure 1 (Hess, 2011; Shane et al., 2016). Patients can experience tenderness, swelling and a decreased range of motion which can limit them to make full dorsiflexion, inversion and eversion during tasks like squatting and descending stairs (Robinson, 2007; Shane et al., 2016). Posterior STI is commonly seen in ballet dancers and soccer player due to the high frequency of loaded plantarflexion. Impingement of this variant is attributed to flexor hallucis longus tenosynovitis, synovitis, impingement of joint capsule and anomalous muscles between the tibia and calcaneus (Yasui et al., 2016; Zbojniewicz, 2019). The inclusion of flexor hallucis longus tenosynovitis is a point of debate however, it is included due to the anatomical location of the tendon sheath within intra-articular structures (Carreira & Ueland, 2020). Patients often experience a deep posterior ankle pain that is hard to accurately locate and can be consistent, sharp, dull and radiating (Yasui et al., 2016). These different types of STI can exist on their own, but also in conjunction with chondromalacia and tendinopathy (Robinson, 2007).
The origin of STI can be insidious or secondary to macro- or microtrauma, which in turn can be acute or repetitive (Carreira & Ueland, 2020; Hess, 2011; Robinson, 2007). For example, ankle impingement is one of two main causes of chronic disability after an ankle sprain, alongside chronic ankle instability (CAI). Approximately 33% of the patients suffering an ankle sprain suffer from pain after a year and 20-39% report chronic complaints after five to seven years (Bestwick-Stevenson et al., 2021). There is a high prevalence of historic ankle sprains within populations of STI (Katakura et al., 2022; Shane et al., 2016). CAI resulting from a sprain, which is developed in 40% of the cases, is also directly related to the development of STI (Hess, 2011; Maffulli & Ferran, 2008; Miklovic et al., 2018). However, the extent of instability cannot simply be attributed to the amount of ligament ruptures involved, but more ligament damage does contribute to a worse clinical outcome due to collateral damage on surrounding tissues (Pacheco et al., 2021). Failed healing after ligamentous damage from, among others, a sprain can lead to hypertrophic fibrosis and altered joint biomechanics. This can lead to friction and entrapped joint tissues (Carreira & Ueland, 2020; Shane et al., 2016; Watson, 2007).
Initial treatment of STI is advised to be conservative. A majority of the patients respond well to combinations of physiotherapy, relative rest / activity modification, bracing / taping, heel-lift orthotics and when indicated corticosteroid injections (Carreira & Ueland, 2020; Hess, 2011; Nery & Baumfeld, 2021; Robinson, 2007; Shane et al., 2016; Watson, 2007; Yasui et al., 2016; Zbojniewicz, 2019). The specific figures of what constitutes a majority, is scarce. Yasui et al. (2016) mention 60% and a case series of footballers concluded that 69% of the players had a successful conservative treatment (Carreira & Ueland, 2020). Most studies do agree that the timeline for a successful conservative rehabilitation should between around three to six months before considering surgery (Carreira & Ueland, 2020; Hess, 2011; Shane et al., 2016; Yasui et al., 2016).
Given the fact that ankle injuries can have a very persistent character and conservative management of STI might have a 60% positive predictive outcome, it is important to go through a thorough examination and make a detailed treatment plan, which extends beyond the ankle joint, to give the client the best chances for recovery. Higher, longer and earlier peroneus longus muscle activation patterns, with longer reaction times, have been observed together with lower tibialis anterior responses as compensatory strategies (Gribble, 2019; Labanca et al., 2021). In regard to proximal joints; strength deficits in the quadriceps, hamstrings and glute muscles are commonly observed, and higher hip/spine muscle activity is present to compensate for the lack of stability. These patterns are present during simple single leg tasks, but also during landing and hopping tasks. During which there is a reduced knee flexion and a more upright spine (Chan et al., 2022; Gribble, 2019; Labanca et al., 2021). Ankle plantar flexors increase their activity to increase landing stiffness and reduce stability related stress (Chan et al., 2022). These consequences also affect the uninjured limb (Ziabari, Haghpanahi, et al., 2022; Ziabari, Razi, et al., 2022).
In regard to the contribution of physiotherapy in the conservative management of STI, studies often mention general domains that should be included, but don’t prescribe specific programs. Physical therapy to improve range of motion, proprioception, strength training of surrounding ankle musculature and specifically peroneal structures are mentioned in multiple studies (Hess, 2011; Shane et al., 2016; Zbojniewicz, 2019). Hess (2011) advises to enhance this rehabilitation with mobilization techniques and sport-specific training. Chan et al. (2022) also pointed out that treatment should focus on increasing available ankle dorsiflexion and knee flexion to evenly distribute forces after landing. Because CAI is directly related to STI, as mentioned earlier in this article, it is of added value to take a closer look at interventions that restore ankle instability.
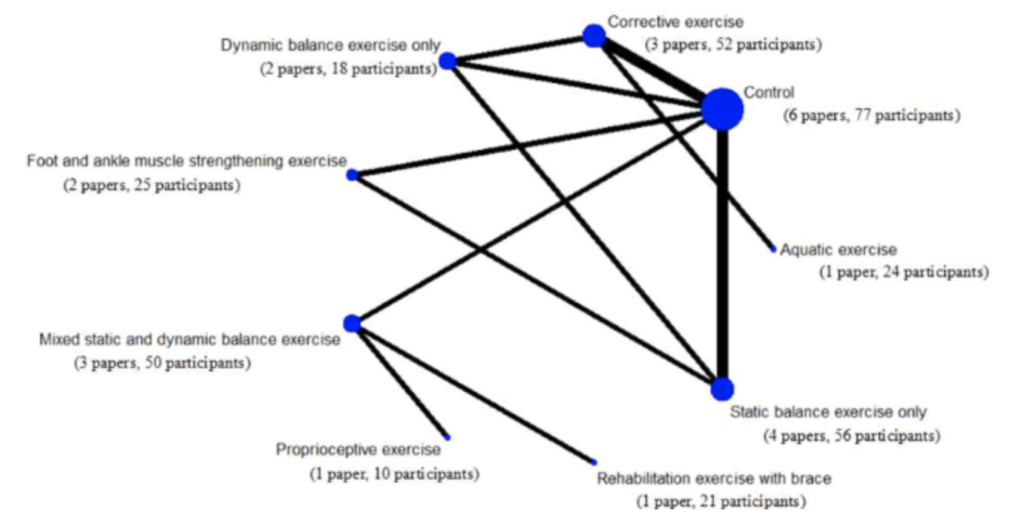
A meta-analysis by Thompson et al. (2018) specified that strength and conditioning of the ankle within populations of CAI should focus on; balance, proprioception (especially passive joint position sense), reaction time and strength deficits. With strong effects for dynamic balance (‘time to stabilization’), peroneal reaction time (especially around 30o of inversion) and eversion strength. Which were the same focal points of Miklovic et al. (2018) to restore postural control in a narrative review describing ‘a pathway of dysfunction’ in the development of CAI. This shows, together with additional publications that functional stability is dependent on multiple variables like inversion/eversion strength, dorsiflexion range of motion and knee strength (Liu et al., 2022). To improve proprioception, the authors of a recent meta-analysis concluded that the best intervention is foot and ankle muscle strengthening followed by static balance training as opposed to dynamic balance exercise, figure 2 (Han et al., 2022). The higher the complexity of the exercise, the worse the effect was to improve proprioception. The rationale why strengthening exercises gave the best result were attributed to: strong afferent stimulation of muscle spindles and cutaneous, capsular, articular and ligamentous receptors with high volume and intensity during the training. Which then results in adaptations to better react to changes in surface, foot placement and increased stability. A second mechanism of improved proprioception was the consequences of healing of damaged mechanoreceptors through enhanced blood circulation, nutrient absorption and metabolism following muscle strength training. Balance training should definitely be added as well, because this improves dynamic balance, instability and functionality (Mollà-Casanova et al., 2021). With the former being an important variable in the rehabilitation of CAI and when present in a STI patient, for these as well (Thompson et al., 2018).
The role of manual therapy in the rehabilitation of STI is not clearly defined. Only Hess (2011) and Chan et al. (2022) describe the possibility of mobilization techniques with STI, but it is not specified how or when to apply this method. A specific search in the scientific databases, regarding STI and manual therapy, doesn’t provide any further answers. Taking a closer look at biomechanical and neurophysiological mechanism in relation to manual therapy in general and specifically the ankle can provide us with some direction based on biologically plausible contentions. It is known that the joint biomechanics are altered in STI due to ligament damage after trauma (Carreira & Ueland, 2020; Shane et al., 2016; Watson, 2007). Capsuloligamentous structures facilitate the axis of rotation and direct forces within a joint (Egmond & Schuitemaker, 2009; Oonk, 1988; Riezebos, 2006). When these are disrupted, for example the Bassett ligament, which happens in STI, the mobility of the talus may get restricted during dorsiflexion and can lead to an anterior subluxation and internal rotation, together with a displacement of the fibular to anterior and inferior (Gribble, 2019; Terada et al., 2013). The model of mechanisms of manual therapy describes that the mechanical stimulus of a mobilization can decrease spasms and increase range of motion (Bialosky et al., 2018). In part, this can be attributed to the generation of piezoelectric tensions within the ligament, leading to restoration of glycosaminoglycans within these structures and as a result; normal tension of the ligaments to maintain proper joint biomechanics (Riezebos, 2006). Mobilization with movement appears to have a positive effect on range of motion when clients have experiences ankle trauma, figure 3 (Hidalgo et al., 2018; Weerasekara et al., 2020). And in regard to chronic ankle instability after trauma, using manual therapy does positively influence outcome measures in fifty percent of the cases (Wikstrom & McKeon, 2017).
This biomechanical reasoning however, is only a small part of the manual therapy model (Bialosky et al., 2018). In particular, neurophysiological mechanisms are the main contributor to positive effects. In the periphery, it can positively influence inflammation mediators and alter inflammation response to exercise. On a spinal level, the bombardment of afferent sensory input from proprioceptors can lead to hypoalgesia, reduced activity of the dorsal horn and modulation of motoneuron pool activity. Finally, manual therapy can lead to reduced activity of supraspinal regions, changes in autonomous responses and increased dopamine production. This can help reduce fear, catastrophizing and kinesiophobia. A recent systematic review concluded that six sessions of manual therapy can lead to improved functional outcomes in combination with functional training within populations suffering CAI (Shi et al., 2019). Not only could this increase the range of motion, it also improved dynamic balance and motor control through afferent proprioceptive input in local joint and nerve structures. The reasoning from their conclusion is in line with the aforementioned model. Walsh, et al. (2020) also recommended to incorporate manual therapy to improve patient-reported outcome scores for patients with CAI in a critically appraisal. Contrary, in a systematic review considering Mulligan’s mobilization techniques on peripheral joints, no benefit regarding range of motion in pathologic ankle injuries could be established (Stathopoulos et al., 2019).
To conclude, STI is a complex and persistent pathology with strong relations to ankle sprains and CAI. An optimal rehabilitation process to maximize the potential of a desired conservative process should be tailor made to the client. The influence of mobility limitations, motor control and capacity of involved tissues should be thoroughly examined. Rehabilitation must consist of specific strength and conditioning exercises and manual therapy might add an additional positive effect, but should be critically considered.


 Soligard, T., Schwellnus, M., Alonso, J. M., Bahr, R., Clarsen, B., Dijkstra, H. P., Gabbett, T., Gleeson, M., Hägglund, M., Hutchinson, M. R., Janse Van Rensburg, C., Khan, K. M., Meeusen, R., Orchard, J. W., Pluim, B. M., Raftery, M., Budgett, R., & Engebretsen, L. (2016). How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. British Journal of Sports Medicine, 50(17), 1030–1041.
Soligard, T., Schwellnus, M., Alonso, J. M., Bahr, R., Clarsen, B., Dijkstra, H. P., Gabbett, T., Gleeson, M., Hägglund, M., Hutchinson, M. R., Janse Van Rensburg, C., Khan, K. M., Meeusen, R., Orchard, J. W., Pluim, B. M., Raftery, M., Budgett, R., & Engebretsen, L. (2016). How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. British Journal of Sports Medicine, 50(17), 1030–1041.